Atkins Health’s Lower Limb Program – Rehab Revolution – is transforming recovery outcomes for Australians undergoing total knee replacement (TKR). While TKR recovery is a key focus, the program is part of a broader lower limb rehabilitation initiative supported by a multidisciplinary team. In addition to physiotherapists and exercise physiologists who lead the TKR program, clients benefit from the expertise of podiatrists, remedial massage therapists, and dietitians. This comprehensive team approach ensures seamless rehab, guiding clients from hospital to their return to work, sport, and the activities they enjoy.
The goal is not just to recover, but to exceed prior levels of health and fitness. By providing ongoing, individualised care that reduces readmissions, the program breaks the cycle of hospital dependency and empowers participants to achieve lasting results.
What is Total Knee Replacement?
Why is it Necessary and How is it Performed?
 Total knee replacement, or total knee arthroplasty, is a surgical procedure designed to relieve pain and restore function in severely diseased knee joints. Most often, this surgery becomes necessary when conservative measures such as medication, injections, and physiotherapy no longer provide relief from debilitating knee pain caused by osteoarthritis, rheumatoid arthritis, or traumatic joint injury.
Total knee replacement, or total knee arthroplasty, is a surgical procedure designed to relieve pain and restore function in severely diseased knee joints. Most often, this surgery becomes necessary when conservative measures such as medication, injections, and physiotherapy no longer provide relief from debilitating knee pain caused by osteoarthritis, rheumatoid arthritis, or traumatic joint injury.
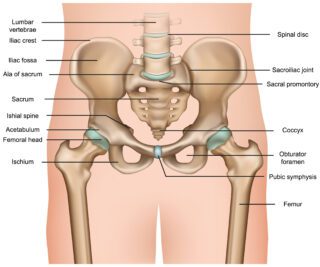
The surgery involves replacing the damaged articular surfaces of the femur, tibia, and patella with prosthetic components made of metal and polyethylene. These artificial joint surfaces mimic natural motion while reducing bone-on-bone contact and inflammation. Surgical candidates typically face challenges in mobility and daily activities, with chronic pain being a major driver.
The procedure is generally highly successful, with most patients reporting significant improvements in pain and function, however revision rates ten years after surgery are almost 11% due to infection or poor rehabilitation. Surgery is therefore really just the beginning. True recovery and optimal outcomes are highly dependent on what happens after the procedure.
Candidates for Total Knee Replacement
While TKR was traditionally seen as a solution for older adults with advanced arthritis, it is now increasingly common across a broader spectrum of Australians.
The following groups are potentially likely candidates:
- Ageing Australians: Particularly those over 60 with reduced mobility, joint deformities, or who are pain resistant to conservative treatment
- Recreational Athletes: Long-distance runners, hikers, and cyclists experiencing progressive wear and tear
- Professional Sports Players: Especially those from high-impact sports such as AFL, rugby, or basketball, with recurrent joint damage
- Manual Labourers: Factory workers, miners, tradespeople, and agricultural workers are at high risk due to repetitive strain and load-bearing tasks
- People with Obesity or Sedentary Lifestyles: Excess weight increases stress on joints, often leading to early-onset osteoarthritis
- People with Previous Joint Trauma or Surgeries: Old injuries may progress to chronic degeneration, especially if left untreated
By identifying and targeting these populations, early intervention and a robust rehab plan can prevent long-term disability.
The Benefits of Participating in the Rehab Revolution Program (and the Risks of Not)
Engaging in a comprehensive, professionally guided rehab program post-TKR is not a luxury, it is a medical necessity.
Benefits of the Rehab Revolution Program:
-
-
- Faster recovery time and return to daily activities
-
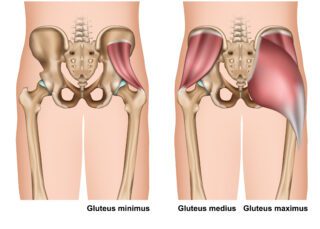
- Improved strength, balance, and mobility
- Reduced pain and swelling
- Lower risk of complications such as deep vein thrombosis (DVT) and joint stiffness
- Psychological benefits, including improved confidence, motivation, and mental wellbeing
- Long-term protection of the prosthetic joint, ensuring greater lifespan and performance
Risks of Not Participating in Structured Rehab:
- Prolonged pain and delayed healing
- Risk of joint stiffness and poor prosthetic integration
- Muscle wasting and functional decline
- Increased likelihood of hospital readmission
- Higher risk of falls and reduced independence
The difference between a mediocre and a life-changing surgical outcome often lies in the quality and consistency of rehabilitation.
Benefits of Our Program:
Stages, Duration, and Professional Collaboration
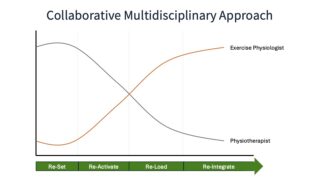
The Rehab Revolution program is designed with both structure and flexibility to support a successful recovery. Spanning 12 weeks, it leverages a collaborative multidisciplinary model involving physiotherapists and exercise physiologists who work closely with your surgeon and care team.
Program Breakdown:
4 x Physiotherapy Sessions (Weeks 1, 2, 4, 8)
- Early-stage recovery focus: joint mobility, pain management, manual therapy
- Progressive restoration of walking and functional movement
1 x Exercise Physiology 1:1 Session (from Week 6)
- Tailored assessment to initiate strength and endurance programming
- Focused on re-activation and neuromuscular control
Weekly Access to Group Classes (Weeks 1–12)
- Supervised, community-based sessions
- Enhances accountability, social engagement, and functional progression
Rehab Stages:
- Re-Set: Post-op pain control, swelling management, reintroduction of movement
- Re-Activate: Early mobility, gait training, baseline strength
- Re-Load: Targeted loading of knee structures, introduction of resistance
- Re-Integrate: Return to full function, advanced balance, and community activities
Throughout the stages, the role of each professional evolves:
Physiotherapist: Takes the lead in the early stages, addressing swelling, mobility, and immediate post-op concerns.
Exercise Physiologist: Increases involvement as functional strength and endurance become the focus, helping maintain progress into long-term outcomes.
Expected Outcomes:
What Makes Atkins Health’s Rehab Revolution Unique
With consistency, participants can expect:
- Notable improvements in mobility and pain within the first three months of structured rehabilitation
- Increased confidence in walking, stair climbing, and daily activities
- Greater independence and reduced reliance on medication
- Improved mood, mental resilience, and social re-engagement
What makes the Rehab Revolution program unique is:
- Close coordination with your orthopaedic surgeon
- A structured, team-based approach, with defined handover points between physiotherapist and exercise physiologist
- Ongoing support, including personalised group training in a welcoming, social environment
- Evidence-based progression, aligned with physical therapy best practices and behavioural science
- Focus on lasting change, not just temporary recovery
This program was developed by experts in physical rehabilitation who understand that recovery is both physical and psychological. By embedding behavioural strategies, personalisation, and outcome tracking, it ensures that each client not only recovers but thrives.
Forget the One-Size-Fits-All Approach:
Whether you’re chasing grandkids, returning to the job site, or getting back on the field, our Rehab Revolution for Total Knee Replacement is your path to a better recovery.
Don’t settle for basic rehab. Choose the program that helps you surpass your previous level of health and fitness – and walk confidently into your next chapter.
Contact us today to learn more or to book your pre-surgery assessment and post-op program, by calling 07 3177 7779 or completing the following form: